Tuberculosis (TB) is a potentially serious infectious disease caused by bacteria (Mycobacterium tuberculosis) that mainly affects the lungs. Though a quarter of the world’s population is infected with tuberculosis bacteria, only a small proportion of those infected become sick with TB. Those with weakened immune systems such as people living with HIV, malnutrition or diabetes, or people who use tobacco, consume alcohol, etc. are at a higher risk of falling ill from TB.
Though the disease is curable and preventable, millions fall ill globally every year across countries and age groups. Over the years, multiple initiatives have been taken at the global level to tackle the disease.

Recently, the World Health Organization (WHO) published the Global Tuberculosis Report 2021 which is an annual publication being published since 1997. The report provides a comprehensive and up-to-date assessment of the TB epidemic and is based primarily on data gathered by WHO in annual rounds of data collection. In 2021, data reported by 197 countries and territories which account for more than 99% of the world’s population and TB cases have been considered.
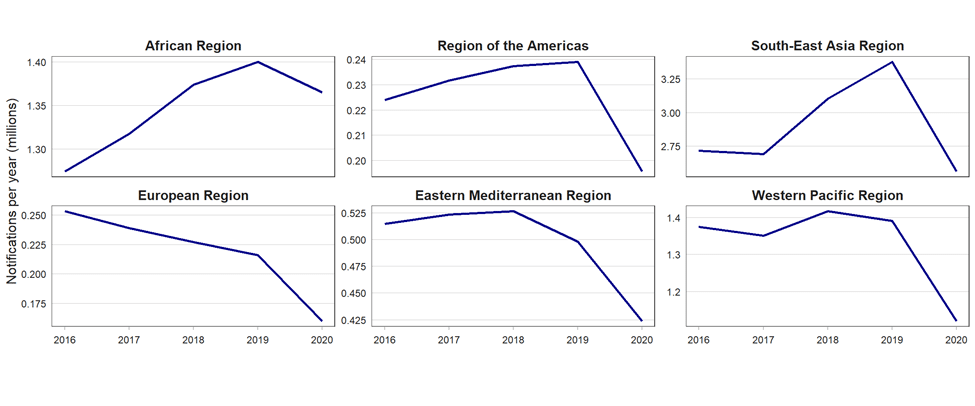
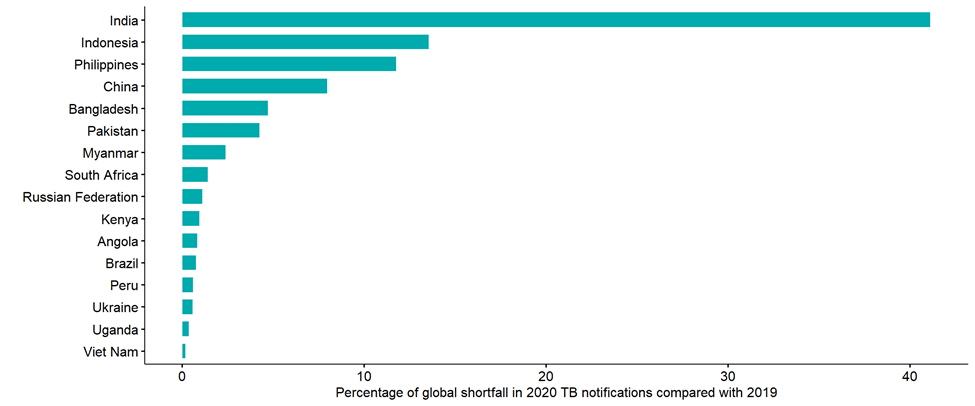
The coronavirus (COVID-19) pandemic has caused enormous health, social and economic impacts in 2020 and 2021. This includes impacts on the provision of and access to essential tuberculosis (TB) services, the number of people diagnosed with TB and notified as TB cases through national disease surveillance systems, and TB disease burden (incidence and mortality). The World Health Organization’s (WHO’s) Global tuberculosis report 2020 included provisional estimates of the impact of disruptions to health services caused by the COVID-19 pandemic on the number of global TB deaths in 2020 and beyond, provisional data on TB notifications in the first 6 months of 2020 and data about response strategies implemented by national TB programmes (NTPs).
COVID-19 has affected TB diagnosis and treatment in India
Similar to the global trend, the number of new cases of TB reported in India in 2020 is less than in 2019. The number of new cases of TB dropped from 2.64 million in 2019 to 2.57 million in 2020, a reduction of 3%. In other words, India reported about 70,000 fewer cases in 2020 compared to 2019 which may be attributed to the effect of the pandemic.
The number of deaths due to TB, including those with HIV, has increased from around 0.45 million persons in 2019 to 0.5 million persons in 2020, an increase of 10%. This trend is on par with the global trend, indicating that India, just like most other countries, has been hit significantly by COVID-19 in providing diagnosis, treatment, and spending.
To control TB spread, it is necessary to prioritise early diagnosis, isolation, and treatment of TB patients so that they don’t become super-spreaders and secondary cases are avoided. However, the disruption of TB programs for the highly vulnerable populations such as poor, marginalised people and restrictions to personal mobility combined with diagnosis delay have negatively impacted vulnerable populations and increased household transmission.
Further, the similarities between TB and COVID-19 symptoms have hindered the detection of TB, leading to misdiagnosis, which we suspect will have an impact on community transmission.

Solutions
If the report gives an impression that 2020 took us decades back in progress against TB, the worst is yet to come. Amid a pandemic, India needs a well-defined strategy in line with the pandemic control to contain, control and treat this infectious disease. Some of the measures that could be taken are:
- leverage the expertise and experience of NTPs, especially in rapid testing and contact tracing, for the COVID-19 response;
- maximize remote care and support for people with TB by expanding the use of digital technologies;
- minimize the number of visits to health services that are required during treatment, including through the use of WHO-recommended, all-oral TB treatment regimens and community-based care;
- limit the transmission of TB and COVID-19 in congregate settings and health care facilities by ensuring basic infection prevention and control for health staff and patients, cough etiquette, and patient triage;
- support the provision of TB preventive treatment by building synergies with contact-tracing efforts related to COVID-19;
- provide simultaneous testing for TB and COVID-19 for individuals when indicated, including by leveraging TB laboratory networks and platforms; and
- ensure proactive planning and budgeting for both conditions (including for the catch-up phase), procurement of supplies and risk management.
The fight against Tuberculosis is a long and sustained one. Public Health issues can’t be tackled in silos. They need an interdisciplinary approach to a problem without hampering the bother programs because every obstacle or pause in Public Health practice takes us back to years in the progress achieved. We can’t undo the efforts in eliminating TB.
Also Read: What is the “mix-match” of Covid-19 vaccine boosters?
















